A growing body of research is forcing scientists to rethink what causes one of the most common infections in the United States: urinary tract infections (UTIs). While UTIs have traditionally been viewed as a personal or hygiene-related health issue, a new study suggests they may also be quietly emerging from America’s kitchens.
Researchers at George Washington University have found strong genetic links between bacteria found in retail meat products and bacteria responsible for thousands of UTI cases across the country. According to microbiologist Lance Price, this connection points to a wider food-safety concern than previously recognized.
“Your risk of infection should not depend on your ZIP code,” Price noted, highlighting how the problem appears to hit low-income neighborhoods harder.
Low-Income Communities Face Higher Risk
The study found that individuals living in economically disadvantaged areas face up to 60% higher risk of foodborne UTIs. Researchers believe several factors may play a role, including limited access to fresh food, fewer meat-safety education resources, and older kitchen infrastructure.
What’s Causing the Infections?
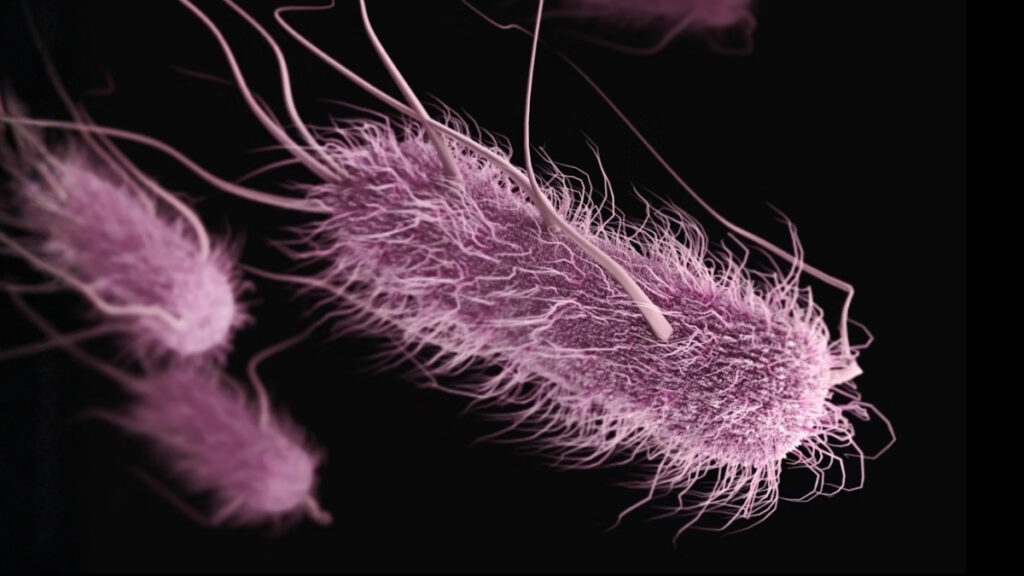
The primary culprit behind most UTIs is Escherichia coli (E. coli). While E. coli exists naturally in the body, certain strains are pathogenic. Bioinformatician Maliha Aziz and her team examined more than 5,700 E. coli samples collected between 2017 and 2021 from both patients and raw meat sold in stores.
After comparing the genetic signatures, up to 20% of the UTI-related bacteria were traced back to animal-origin foodborne strains.
Poultry products — and turkey in particular — showed the highest contamination levels.
How the Spread Happens
Contamination can easily move from raw meat to:
Countertops
Cutting boards
Kitchen utensils
Hands
Even small lapses in sanitation can allow bacteria to survive long enough to cause an infection days later.
Safe-Handling Guidance
The U.S. Department of Agriculture and the study’s authors recommend:
Keep meat securely sealed during transportation
Prepare raw meat last, after handling produce
Use a separate cutting board for raw meat
Do not wash raw meat (it spreads bacteria through splash)
Wash hands with soap for at least 20 seconds after contact
Use a food thermometer:
Poultry: 165°F (74°C)
Ground meats: 160°F (71°C)
Whole cuts: 145°F (63°C)
Millions Impacted Every Year
UTIs are among the most common bacterial infections in the U.S., particularly affecting women. Recurring cases can be debilitating, and misdiagnosis often leads to unnecessary antibiotic use — contributing to the growing concern of antimicrobial resistance.
A National Problem, Not Just One State
While the research was conducted in California, scientists believe the issue is nationwide. Meat distribution networks are interconnected, and food-handling habits tend to be similar across states.
More Research Needed
The study, published in the journal mBio, calls for expanded investigation into:
Slaughterhouse hygiene
Transportation conditions
Retail storage practices
Community food-education gaps
Price argues that this issue highlights broader social determinants of health — including income, education, and local infrastructure.
“This opens up new avenues for prevention,” he said. “It’s a reminder of why we should be investing more in public-health research, not less.”
What’s Next
Public-health experts say that until stronger controls are in place, consumers must rely on safe-handling habits at home. Meanwhile, policymakers may face growing pressure to address disparities that allow foodborne infections to hit some communities harder than others.